Thinking about how we will be spending the coming summer might feel premature at a time when coronavirus cases are soaring throughout Europe and America. The current situation appears like January 2020 all over again: New mutations of SARS-CoV2 that have emerged in Great Britain, South Africa, and Brazil and are threatening to take most of the Western world by surprise, with strained healthcare systems and overwhelmed governments woefully unprepared to avert the danger of an unmitigated spread.
Now, one might be convinced that the end of the dark is near: vaccines are on the way and the warmer weather will make it much easier to get back to a more normal way of living. While not necessarily false, it would be unwise to rely on those things alone. Some countries, like Israel, are on the way to having vaccinated most of their citizens by early-to-mid summer. But most of the developed world will only be able to supply a vaccine to the most vulnerable by then, and any major hiccups, like production losses, delays in vaccine approval, or vaccine-evading mutations, might set us back in the goal of ending the pandemic. It is also still not entirely clear if people who are vaccinated can still transmit the virus to others, though initial studies suggest that some vaccines significantly reduce infectiousness. Many developing countries will not have any meaningful access to vaccines until 2022, instead having to rely on traditional measures like social distancing, testing & tracing, and masks. While the warmer weather certainly helps in some circumstances, it is not going to save us by itself, as the recent situation in South Africa, Brazil and Los Angeles clearly shows.
What does this mean for live music? From a public health perspective, a live concert is one of the worst places to be during a pandemic. A guideline from Japanese health authorities advises to avoid the 3 C’s: closed spaces with poor ventilation, crowded places with many people nearby, and close-contact settings such as close-range conversations. A sold-out show in a small, busy bar ticks all three of those boxes: a lot of people crammed together in a small, poorly ventilated room, drinking alcohol, chatting and singing along to the music, are bound to produce lots of potentially infectious particles.

Standing in line for an overcrowded bar gig? That’s unlikely to happen anytime soon. (Photo by Rade Zivanovic)
We know this because of super-spreader events that occurred in much more mannered settings. In March of 2020, a group of 61 people in Skagit County, Washington convened for a two-and-a-half-hour choir practice. Among them was one person with cold-like symptoms. The practice led to 53 infected people, of which three had to be hospitalized and two died. After a practice session of the Berlin cathedral choir, 62 of the 82 participants were infected with the coronavirus despite social distancing. While scientists still debate the precise pathways of transmission — singing, coffee breaks, ridesharing, or others—what these examples show us that the concert experience we are used to will have to be modified to be safe.
That’s because concerts draw their crowds from different cities, often younger people, who are both more mobile and less likely to develop obvious symptoms, if any. It’s incredibly difficult to warn these people before they infect their housemates, families or colleagues. But while COVID-19 is particularly dangerous for the elderly, younger adults can also be severely affected: around one in a hundred need to be hospitalized, around one in ten suffer from ongoing symptoms like fatigue, shortness of breath or headaches. Heart damage affects not only older patients, but also young, healthy athletes with mild or even asymptomatic cases of COVID-19. So how can we make sure that a concert does not trigger a region-wide outbreak? There are three basic ways.
First, we can try to ensure that no infectious persons are present; second, we can attempt to reduce or eliminate the infection risk at the venue; and finally, we can try and mitigate the damage when it is already done.
Nothing spreads without someone to spread it
Consider this simple example. Let us assume there was a sold-out concert held tomorrow at the biggest permanent indoor concert hall in Cologne, which has a capacity of 4000. At the current incidence of the coronavirus in Europe, we would expect between two and ten of these people to be currently infected. Unfortunately, there is no easy way to find those people within the crowd. Testing 4000 people via PCR would not only be too costly, it would also take at least half a day to get all those test results back. Rapid tests are a way around this problem, but they come with their own sets of issues. For the simplicity of the argument, let’s assume that we expect ten infected people to be in our crowd of 4000.
It’s helpful to understand the course of infection in order to understand the logic behind rapid tests. When someone is infected, it usually takes around five days to develop symptoms like fever, dry cough, loss of smell and taste, or fatigue. (Some people, especially children, might never develop symptoms at all.) Their viral load peaks around that time, too, which is a huge problem — they become infectious about a day before they notice they’re sick. In these early stages, a day sooner or later makes a huge difference. After that, the viral load slowly decreases, until after about ten days, they are no longer infectious.
Unlike PCR tests, which can find even tiny amounts of viral genes left after two weeks, rapid tests are less sensitive — they detect between a third and a half of those who are infected. What sounds like a downside is actually an upside: we are not interested in those who had the infection three weeks ago, but in those who have high viral loads and are highly infectious right now. Rapid tests help us catch these infectious people, detecting about 80 to 100 percent of those with high viral loads. In our example, a rapid test might find four out of ten infected visitors while missing the other six, which we would assume not to be currently infectious.
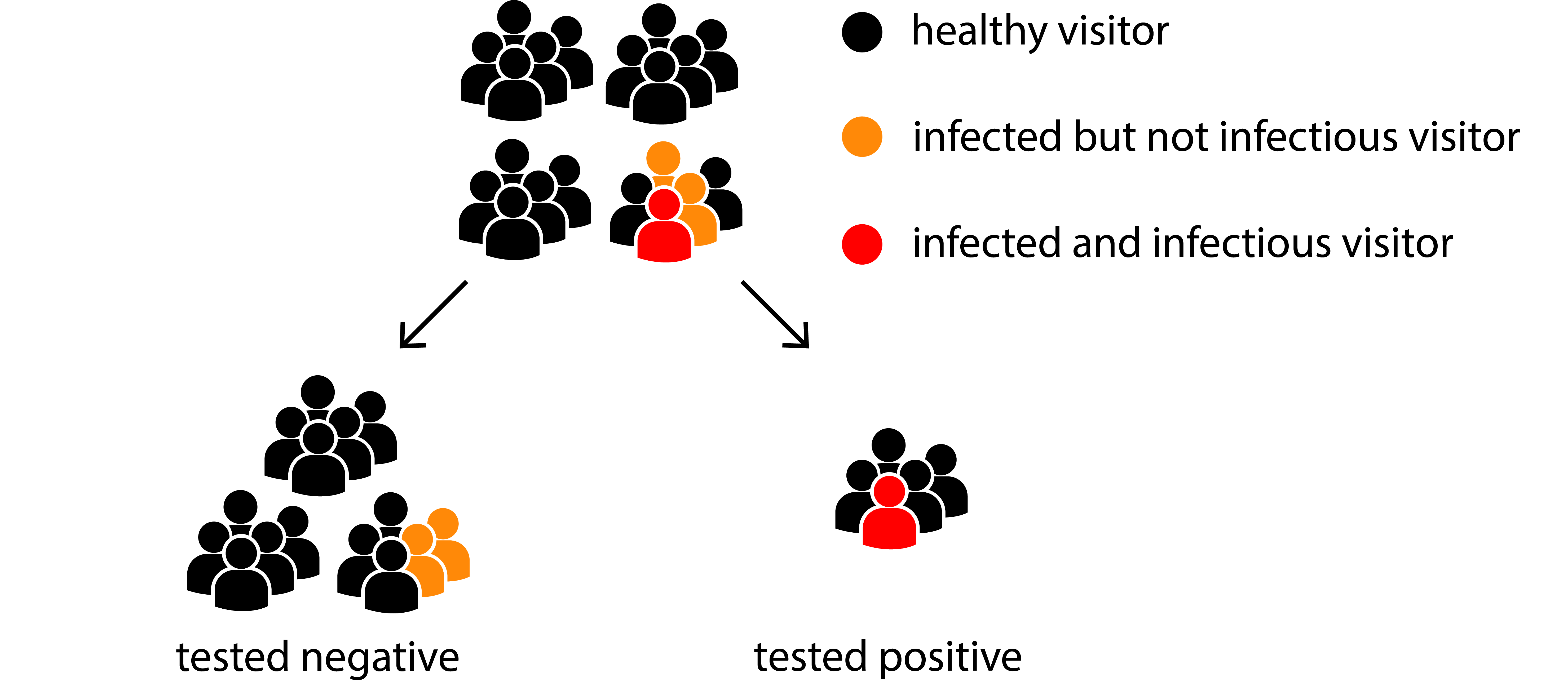
The idea behind testing: we are looking for those who are infectious, not for those who are sick.
What if I get tested right now and get a negative result? In short, there are three possibilities: I am healthy; I am infected, but am no longer infectious; I am infected, but have not yet gotten sick. In the last (and worst) case, you might become infectious tomorrow, so you should not trust a result that is older than a day. If the sample is not taken properly, there is a fourth possibility: you are infectious, but there was not enough viral antigen in the sample to detect it. If that happens in our example above, some of the four infectious visitors might get a false negative result, so we shouldn’t trust rapid tests blindly. Researchers are still debating what way of swabbing people yields the most reliable results — the established way, sticking a swab all the way to the back of the nose is uncomfortable and takes some practice.
But what if you test positive? Most rapid tests correctly identify over 99% of healthy people as negative. That sounds very good, but in our example above, 20 people would falsely be detected as positive although they are healthy. What’s more, those who are false positive will get tested positive all the time, because they naturally have bacteria in their mouth that trigger some of the rapid tests. It’s unfortunate, but in that case, you would get a refund and be sent home to isolate until your doctor can perform a PCR test.
There’s another very primitive way to reduce the danger of infectious people being present: reducing crowd sizes. If we were to split our 4000-people event into 20 separate concerts, the ten infected people would be diluted so much that only two of the concerts would be visited by an infectious person. What’s more, half of the concerts wouldn’t have any infected visitors at all. Testing everybody would bring us a long way to having safer concerts for concert goers as well as for musicians and other staff, where regular testing is easier to implement and even more effective. And whoever gets tested positive need not necessarily worry: in our example, only one sixth of them would really be infected.

The effect of splitting a crowd into smaller groups: in three of four crowds, there are no infectious visitors.
Keep away from bad air
It’s really the few remaining occasions that all the other measures are there for and most are relatively easy to understand and follow: wear a (well-fitting) mask, keep your distance from other people, and wash your hands. It’s when we move indoors that it starts to get complicated.
When public health officials began advising mask-wearing and social distancing, it was based on the assumption that the coronavirus spreads through heavy droplets we shed while speaking, singing or sneezing and which hit our eyes, nose, mouth, or surfaces we touch frequently. Over time, scientists in east Asia found transmission situations where this theory seems implausible. In South Korea, researchers examined a restaurant where two guests contracted the virus from an infectious visitor sitting on the opposite side of the room. By inspecting camera footage and measuring air flows within the restaurant, they concluded that air conditioning had picked up breathing air from the infectious guest and blown it onto the two people who later got sick. Their companions, who were not sitting within the air stream during those ten minutes, were not infected. Recent transmissions in Australian quarantine hotels show that the coronavirus and especially its mutated variants are insidious in using the tiniest opportunities to spread.

A graphic representation of the restaurant where two visitors got infected by air flow. J Korean Med Sci. 2020 Nov;35(46):e415. © 2020 The Korean Academy of Medical Sciences.
Every breath, cough, or sneeze contains tiny water particles that can contain the coronavirus. While bigger ones eventually sink to the ground, others, called aerosols, are so small that they float through the air. An infectious person creates a cloud of these potentially contagious aerosols around themselves that slowly gets diluted by the air around it. The exact dose needed to infect a person is still unknown, but it can quickly accumulate in a closed room. Hence, keeping distance from others is very important, but it is not enough.
The breathing air of an infected person is exemplified by stage smoke here. Although some smoke passes around the mask, it is quickly removed by the ventilation system. Most aerosols are much bigger than the smoke particles in this video and thus are filtered by the mask.
No shoes, no mask, no service
Face masks are another layer of protection we cannot do without. When worn by the infected person, they not only catch most of the bigger droplets, but also filter out some of the smaller aerosols. However, they can protect a healthy person from infection, too, as a basic surgical or multi-layered cloth mask still filters out between one and three fourths of all particles we inhale through breathing. The fit is almost as important as the material, though: any mask is of little use if the air just passes through the gaps around your nose and cheeks. Another problem with masks is that they lose their protective effect when they get wet, especially when worn continuously for several hours. Finally, it’s impossible to have a drink with a mask on — a problem because selling drinks is an important source of income for most venues.
That’s why moving concerts outdoors is such an obvious way to reduce risk. Small clubs are tricky because narrow corridors and crammed spaces make it difficult to socially distance, while usual ventilation systems might be insufficient to remove the virus from the air. Remember those concerts where the air is stale and sticky and the windows are fogging up? You shouldn’t feel safe there because you aren’t; odors and high humidity are dead giveaways for rooms that lack air exchange. What’s more, the lack of fresh air is often on purpose: the more ventilation, the harder it gets to control noise.
Concert halls and opera houses are a different story. A recent study at the Konzerthaus Dortmund concluded that the risk of infection there is very low if the audience wears masks and is seated in a checkerboard layout. What might seem surprising makes perfect sense: our breathing air is warmer than the air that surrounds us, so that it rises up to the ceiling of the auditorium where dedicated ventilation systems exchange the entire air within 20 minutes. Also, the sheer room volume of many auditoriums ensures that infectious aerosols are diluted, while the seating prevents infectious people from moving around and mingling in the crowd. The protective environment of the auditorium, however, does not extend to toilets, cloakrooms, entry areas, the queue in front of the venue, or the bus you take to get there in the first place — which might explain the hesitancy of public authorities in allowing large-scale events.
So don’t expect throwing yourself into mosh pits and headbanging in stinky basement clubs anytime soon. The requirements of infection protection instead favour a different kind of setting: seated concerts in big auditoriums or concert halls, with bigger distances between masked visitors; quieter, instrumental, more acoustic settings where doors and windows can stay open; and spacious outdoor locations and open-air stages that have seldom been used in the past.

Philharmonic halls might be among the first places to open back up.
How can we get the genie back into the bottle?
No matter how stringent the safety measures may be, however, some transmissions are bound to happen, which is where swift action makes a big difference. That’s because when somebody is infected with the coronavirus, the clock starts ticking: remember, you can be infectious one or two days before developing symptoms. Anyone who develops a dry cough or fever, loses his sense of taste and smell, or feels tired should take those warning signs seriously and get tested immediately. That way, they not only protect their own contacts, but they may also point health authorities and concert organizers to a bigger problem — if several concertgoers report sick at the same time, they may have gotten infected at the same site, indicating a larger outbreak. In order to move quickly, venues will need digital solutions to handle our contact information and in fact, numerous initiatives are already developing apps to make it easier for everyone involved. Most likely, we will be asked to scan a QR code with our phones and either automatically transfer or manually enter our contact data in an online form. That way, organizers could contact us if visitors end up testing positive.
Depending on how hard the mutated strains of the coronavirus hit us, it might take us until May, June or even July to get to a point where we can safely end the lockdowns and reopen. But we should remember that the tools we have to stay safe during a wave of infections can also help us to make concerts safer during a looming pandemic — and maybe, when all this is over, we might not miss the sweaty t-shirts and stinky crowds after all.